Peyronie’s disease can be caused by various factors, but here are the top 50 reasons associated with its development:
Table of Contents
Definition:
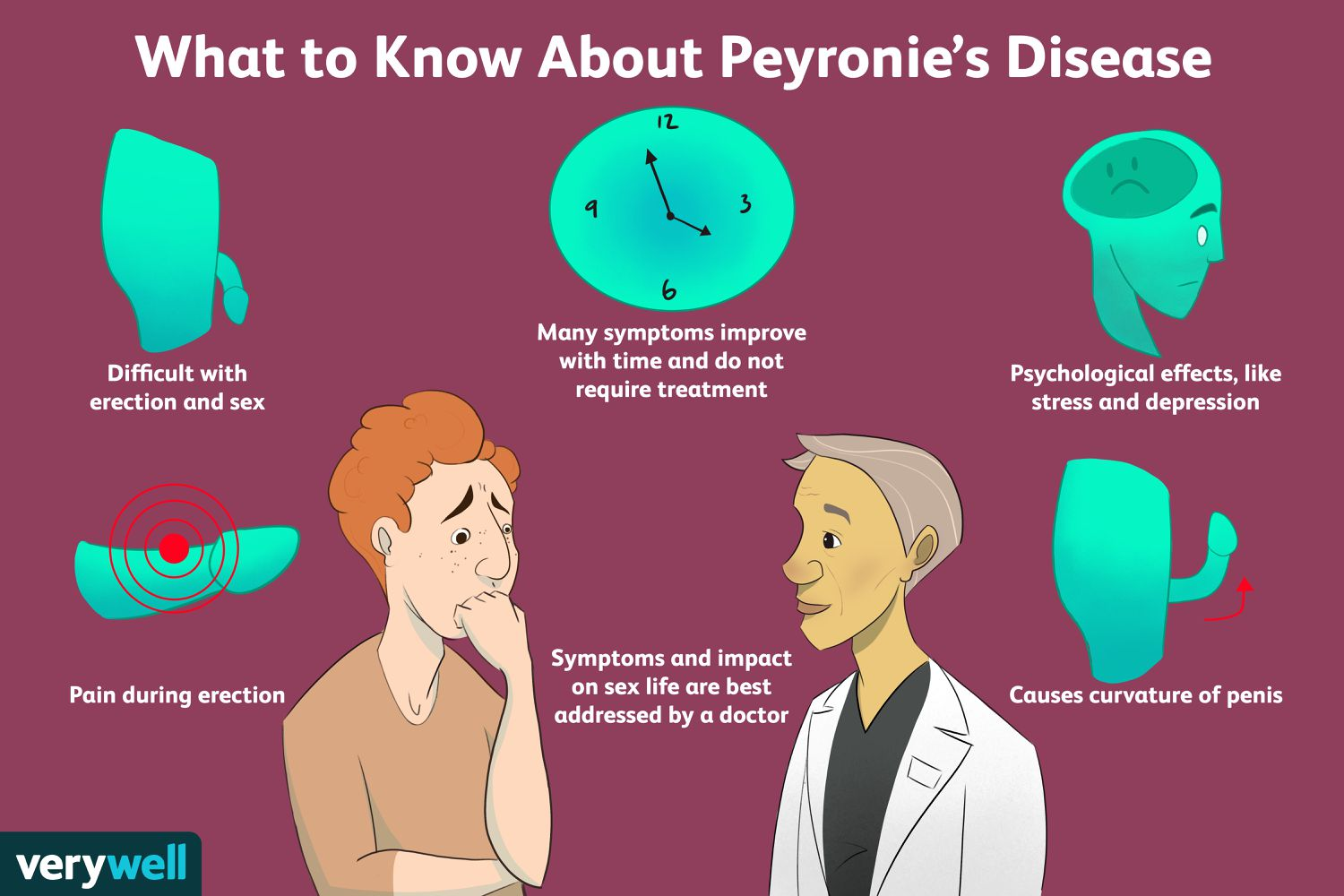
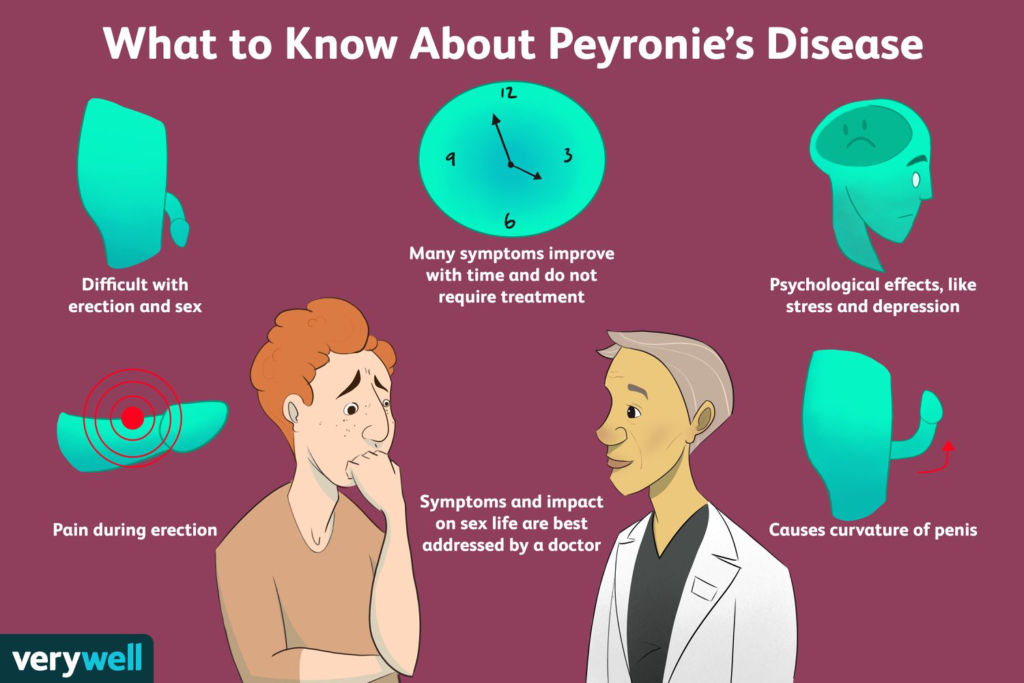
Peyronie’s disease is a condition characterized by the development of fibrous scar tissue inside the penis, causing curvature or bending during erections.
Etiology:
The exact cause of Peyronie’s disease is unknown, but it’s believed to involve trauma or injury to the penis, genetic factors, and inflammation.
Symptoms:
- Penile curvature or bending during erection.
- Pain or discomfort during erection.
- Erectile dysfunction (difficulty achieving or maintaining an erection).
- Shortening of the penis.
- Presence of a lump or plaque under the skin of the penis.
Diagnosis:
- Physical examination of the penis by a healthcare professional.
- Medical history assessment.
- Imaging tests such as ultrasound or MRI may be used to visualize the scar tissue and assess the extent of curvature.
Treatment options:
- Watchful Waiting: In some cases, Peyronie’s disease may resolve on its own without treatment.
- Medications: Oral medications like collagenase injections may help reduce plaque size and improve symptoms.
- Penile traction therapy: Devices that apply gentle stretching to the penis may help reduce curvature over time.
- Penile injections: Injecting medications directly into the plaque may help soften it.
- Surgery: In severe cases where conservative treatments fail, surgical procedures like penile plication (shortening the side of the penis opposite to the plaque) or grafting (adding tissue to the shorter side of the penis) may be necessary to correct curvature.
Complications:
- Erectile dysfunction.
- Difficulty with sexual intercourse.
- Psychological distress, including depression and anxiety, due to changes in appearance and sexual function.
Prognosis:
- The course of Peyronie’s disease varies widely among individuals.
- Some cases may improve or stabilize over time without treatment.
- Others may progress and lead to significant curvature and sexual dysfunction.
Prevention:
- Avoiding trauma to the penis during sexual activity or other activities.
- Seeking prompt medical attention for any penile injury or trauma.
- Discussing any concerns about penile curvature or symptoms with a healthcare provider promptly.
Support:
- Support groups and online forums can provide emotional support and information for individuals living with Peyronie’s disease and their partners.
Follow-up:
Regular follow-up appointments with a healthcare provider are essential to monitor the progression of the condition and adjust treatment as needed.
Top 50 reasons for peyronie’s disease
- Penile trauma or injury, such as during sexual activity or accidents.
- Genetic predisposition or family history of Peyronie’s disease.
- Age-related changes in penile tissue structure and function.
- Autoimmune disorders leading to inflammation and scarring of penile tissue.
- Connective tissue disorders like Dupuytren’s contracture, which can also affect the penis.
- Certain medications, including beta-blockers and antihypertensive drugs, linked to collagen deposition and fibrosis.
- Diabetes, which can cause microvascular damage and impaired wound healing in the penis.
- Hypertension, contributing to vascular dysfunction and tissue damage.
- Smoking, which increases oxidative stress and inflammation, leading to tissue damage and fibrosis.
- High cholesterol levels, promoting atherosclerosis and vascular damage.
- Obesity, leading to hormonal changes, inflammation, and metabolic dysfunction.
- Peyronie’s disease has been associated with certain genetic markers and mutations.
- Chronic inflammation of the penile tissue due to repeated infections or other inflammatory conditions.
- Hormonal imbalances, including low testosterone levels, affecting penile tissue health.
- Occupational hazards involving repetitive trauma or pressure on the groin area.
- Pelvic radiation therapy for prostate cancer or other pelvic malignancies, leading to tissue damage and scarring.
- Substance abuse, including excessive alcohol consumption and illicit drug use, affecting tissue health and healing.
- Prior penile surgery, such as circumcision or penile implants, increasing the risk of scar formation and curvature.
- Peyronie’s disease has been linked to certain viral infections, although the exact mechanisms are not fully understood.
- Hematological disorders affecting blood flow and clotting, leading to compromised penile tissue health.
- Endocrine disorders like hypothyroidism or hyperthyroidism, influencing tissue metabolism and healing.
- Chronic kidney disease, leading to metabolic imbalances and tissue damage.
- Peyronie’s disease has been associated with certain autoimmune conditions like rheumatoid arthritis.
- Inflammatory bowel disease (IBD) like Crohn’s disease, which can involve systemic inflammation and affect penile tissue.
- Penile implants or prostheses, which can cause mechanical stress and inflammation in penile tissue.
- History of priapism (prolonged erections) leading to tissue ischemia and fibrosis.
- Systemic sclerosis or scleroderma, characterized by widespread fibrosis affecting multiple organs, including the penis.
- History of penile injections for erectile dysfunction, which can lead to localized tissue damage and scarring.
- Use of anabolic steroids for bodybuilding, leading to hormonal imbalances and tissue changes.
- Neurological disorders affecting penile sensation and erectile function, contributing to trauma during sexual activity.
- Psychological factors like stress, anxiety, or depression, which can influence sexual behavior and penile trauma.
- Congenital penile abnormalities or deformities, increasing susceptibility to trauma and curvature.
- Presence of penile adhesions or phimosis, which can lead to microtrauma during sexual activity.
- Overuse or misuse of penile traction devices, causing tissue damage and fibrosis.
- Chronic urinary tract infections, leading to inflammation and scarring of penile tissue.
- Certain dietary factors, including high intake of processed foods or saturated fats, affecting tissue health and inflammation.
- Sleep disorders like obstructive sleep apnea, which can lead to systemic inflammation and tissue damage.
- Environmental toxins or pollutants, which can have systemic effects on tissue health and healing.
- Chronic stress or cortisol dysregulation, affecting immune function and tissue repair processes.
- Chronic prostatitis or pelvic inflammatory conditions, leading to inflammation and scarring of surrounding tissues.
- History of sexually transmitted infections (STIs) like gonorrhea or chlamydia, which can cause inflammation and tissue damage.
- Chronic use of certain medications like finasteride (used for benign prostatic hyperplasia), which can affect tissue remodeling processes.
- Use of penile traction or stretching exercises without proper guidance, leading to tissue damage and scarring.
- Presence of metabolic syndrome, characterized by a cluster of conditions including obesity, insulin resistance, and hypertension, which can affect penile tissue health.
- History of priapism-inducing medications like intracavernosal injections for erectile dysfunction.
- Chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), which can impair tissue healing processes.
- Chronic liver disease leading to metabolic imbalances and tissue damage.
- Overuse of recreational drugs like cocaine or methamphetamine, which can lead to vasoconstriction and tissue ischemia.
- Certain dietary supplements or herbal remedies that may have pro-fibrotic effects on penile tissue.
- History of sexually risky behavior or multiple sexual partners, increasing the risk of penile trauma and inflammation.
It’s important to note that while these factors are associated with Peyronie’s disease, not everyone exposed to them will develop the condition, and the exact cause can vary from person to person.
https://impetusgurukull.com/category/us-big-newz/